UGA researchers received prestigious grant to develop malaria drug
by Amy Horton
New compound targets P. vivax, source of recent U.S. infections
Two University of Georgia researchers have been awarded approximately $770,000 from the Global Health Initiative Technology (GHIT) Fund to develop a new drug to kill the dormant liver stages of Plasmodium vivax, the most widespread of the malaria parasites. This amount is part of a total of JPY 334,238,778 awarded by the GHIT Fund to a partnership consisting of UGA, Medicine for Malaria Venture and Mitsubishi Tanabe Pharma Corporation.
“P. vivax often persists in the liver of patients, causing a relapse infection following treatment of the symptomatic blood infection,” said Steven Maher, associate research scientist in the Office of Research’s Center for Tropical and Emerging Global Diseases (CTEGD). “In many parts of the world, relapses account for the majority of total P. vivax cases.”
The announcement comes on the heels of reports of the first locally acquired cases of malaria in the United States in 20 years. In the summer of 2023, seven cases of locally acquired P. vivax malaria were reported in Sarasota, Fla., and one in Cameron County, Texas. These are in addition to a case of P. falciparum diagnosed in a Maryland resident living in the National Capital Region.
Most malaria cases diagnosed in the United States occur in people who have traveled to countries in South America, Africa, and southeast Asia where malaria is endemic. While locally acquired mosquito-transmitted malaria cases can occur, as Anopheles mosquito vectors exist throughout the United States, they are rare. The last reported outbreak was in 2003 when eight cases of locally acquired P. vivax malaria were identified in Palm Beach County, Fla.
The GHIT award will allow Maher and Chet Joyner to develop a compound series drug-screening program. Joyner is an assistant professor in the College of Veterinary Medicine’s Department of Infectious Diseases and Center for Vaccines and Immunology and jointly appointed to CTEGD.
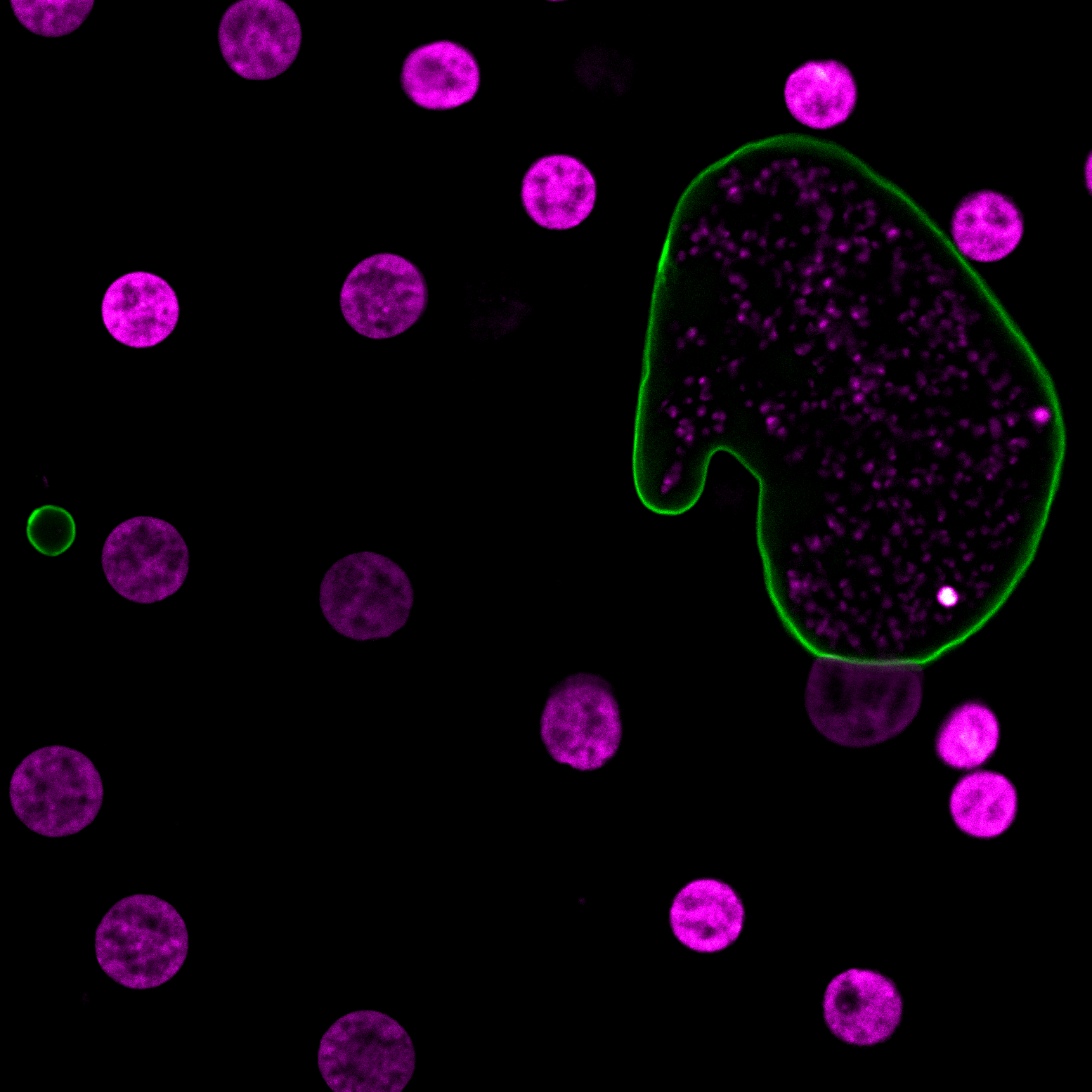
The compound series identified by Maher, the result of testing more than 100,000 samples using infected liver cells, is the first new chemical class discovered in more than 70 years with efficacy against the persisting liver stage. Over the next two years, Maher and Joyner will be collaborating with Medicine for Malaria Venture and Mitsubishi Tanabe Pharma Corporation to alter the chemistry of the compound to improve drug-like properties, including half-life and potency, necessary to achieve single dose criteria.
“Discovering a drug to kill dormant, non-proliferating cells is extremely difficult, yet with the novel assay the team developed we now have the first new target and drug class with potential to accelerate global malaria elimination efforts,” said Dennis Kyle, director of the CTEGD.
The current drug class used to treat P. vivax malaria, 8-aminoquinolines, often results in serious side effects and cannot be administered to pregnant women, who are one of the patient groups most in need of treatment.
“We have the first validated compound that kills vivax while it lies dormant in the liver,” Joyner said. “We hope in the next two years to help advance the new compounds to clinical testing.”
Lisa K. Nolan, dean of the College of Veterinary Medicine, said the work Maher and Joyner are doing could deliver a better quality of life to millions of people around the world.
“This great research is a shining example of our commitment to translational research, which will take this drug from the lab to preclinical testing to the patient rapidly,” Nolan said.
