Outhouses, clean water key to fighting schistosomiasis in persistent hotspots


Schistosomiasis, caused by several species of the parasitic worm Schistosoma, is a disease of poverty. The debilitating illness keeps people in a cycle of poverty due to missed educational and employment opportunities. In children, repeated infections often lead to anemia, malnutrition and learning disabilities. While there are no current preventive drug therapies or vaccines, annual mass drug administration (MDA) is often used to treat all elementary school children in countries where Schistosoma species are endemic.
“Treating with praziquantel through MDA programs is really successful in reducing schistosomiasis,” said Dan Colley, professor emeritus in the Franklin College of Arts and Sciences’ Department of Microbiology and former director of the Center for Tropical and Emerging Global Diseases. “However, in our studies we were seeing a few villages that didn’t really respond to annual MDA with lower numbers of infections. And it wasn’t just a few villages—in any given group of 25 study villages, we saw what we’re calling ‘persistent hotspots.’”
Through the work of the Schistosomiasis Consortium for Operational Research and Evaluation, researchers discovered that persistent hotspots (PHS) occurred in study sites in Cote d’Ivoire, Mozambique, Tanzania, Zanzibar and Kenya.
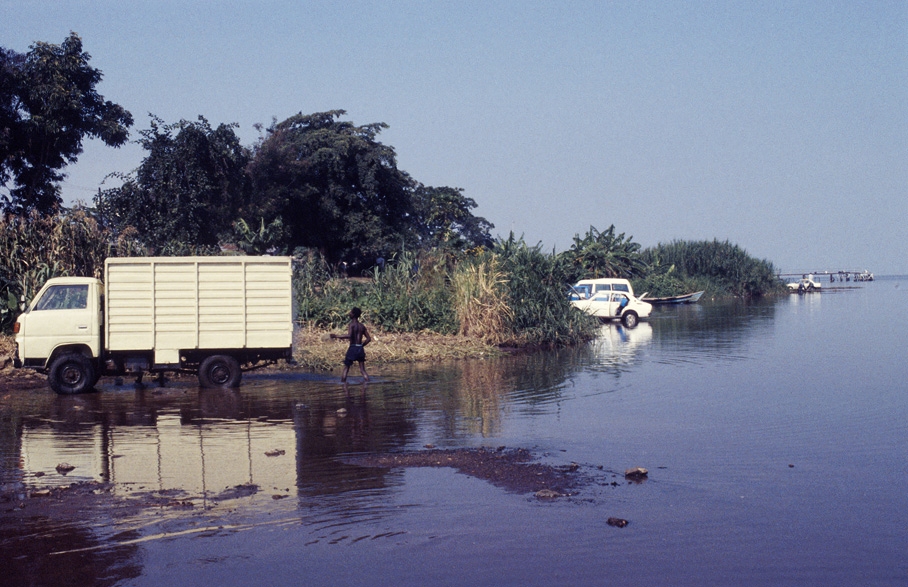
Schistosoma parasites develop in certain species of freshwater snails and are shed into the water where the form of the parasite that infects people can survive up to 24 hours. When an individual comes to the water to bathe, wash clothes, work or play, the parasites invade through the skin.
Several weeks after infection, the worms mature and begin to produce eggs that travel to the person’s bladder or intestines, where they are expelled through urine or stool. When freshwater sources are contaminated with human urine or fecal matter that contain these eggs, the life cycle begins again when the parasite eggs hatch and infect appropriate freshwater snails.
In a recent study published in PLOS ONE, Colley and his colleagues at the University of Georgia, Kenya Medical Research Institute (KEMRI), and Kenya’s Ministry of Health found high use of surface water and low use of latrines were factors associated with being a PHS and likely contributed to persistent levels of Schistosoma infection in these PHS villages—even in the face of annual MDA.

The study in western Kenya included both villages responding well to MDA (with a declining level of schistosomiasis) and those that are considered persistent hotspots. All the villages have fewer than 2,000 people, and most range between 500 and 1,500 residents. They often contain a crossroads that serves as the town center with a few shops. While the town center and the nearby houses have electricity, homes farther out might not. Villages considered PHS were located closer to open water sources, and more residents were employed in water-based jobs such as car washing and sand harvesting.
It was also found that these PHS villages had fewer latrines than villages that responded well to MDA, which likely led to more human fecal matter washing into the surface waters. The researchers believe that for these PHS villages, increasing latrine availability and use would reduce Schistosoma prevalence. However, it isn’t just a case of “if you build it, they will come.”
There are several barriers that would need to be overcome. Latrines, commonly called outhouses, are often smelly and attract flies and rats, which then attract snakes. In addition to issues of maintenance, there are social and educational components that need to be considered to change practices. But even when the people are willing, increased latrine use doesn’t always work.
Colley recounts the story of a group of car washers he and other colleagues at KEMRI and the Centers for Disease Control and Prevention worked with for over two decades. These men are well-versed on Schistosoma, and they decided to build a latrine.
“They knew the life cycle as well as we did, maybe better,” recalls Colley.
The car washers even made it an entrepreneurial pursuit by selling toilet paper for a shilling. However, when the rainy season came, the latrine was flooded, and all that waste was washed into the nearby lake where they worked daily.
This story illustrates just one of the challenges public health officials face in trying to incorporate wells and latrines into national programs to eliminate schistosomiasis. Studies like the one by Colley and his colleagues demonstrate the need to look beyond drug treatment when pushing to move from control to elimination of schistosomiasis.
“We can keep doing MDA, which is helpful, but eventually the worms may become drug resistant,” said Colley. “But with persistent hotspots now being found in everyone’s studies, we know we need to do better. That means we need to advocate for access to clean water sources, sanitation and perhaps ultimately vaccines, as well.”
